Nursing capstones share empirical findings
Wednesday, May 3, 2023
Photos by Jennifer A. Cline, writer/magazine editor
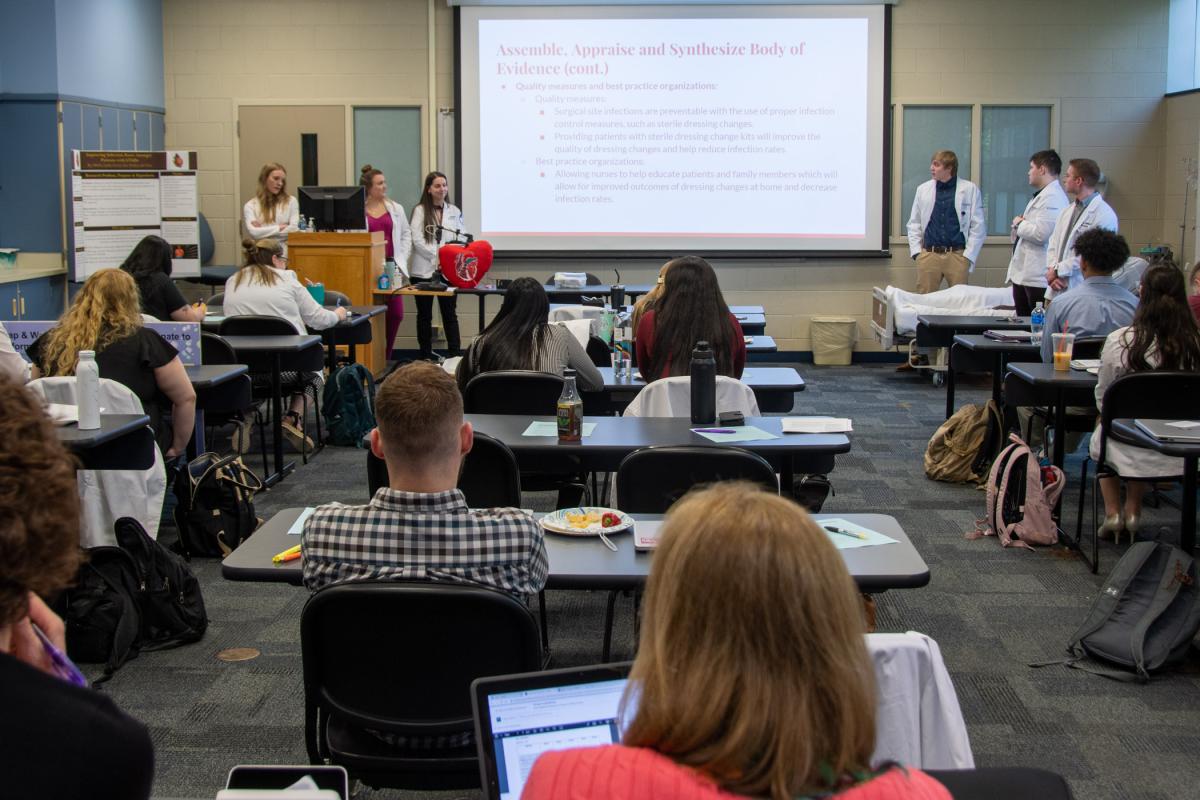
Pennsylvania College of Technology bachelor’s degree nursing students – all slated to graduate this month – recently presented capstone projects that not only tied together their final three courses but also resulted in research-based innovations – some marketable, all usable in critical care settings.
The four student groups presented their work in the classroom and at the Geisinger Nursing Student Scholarship Conference on April 28. The conference comprises research findings from nursing students at six colleges: Penn College, Bloomsburg University, King’s College, Marywood University, Misericordia University and Wilkes University.
The bachelor’s degree nursing major’s May graduating class gathers in front of their Breuder Advanced Technology & Health Science Center home base.
Penn College students’ work started with an observation made during their clinical rotations in the Adult Health Nursing III class, taught by Pamela W. Baker, associate professor of nursing. In Research & Theory in Clinical Practice, taught by Joni J. Pyle, associate professor of nursing, they researched the issue they saw (and, in the process, practiced their skills at accessing and critiquing scholarly literature and developing their own proposals for collecting data). In Leadership & Management in Nursing, taught by Donnamarie Lovestrand, assistant professor of nursing, the students developed a means to change a real-world practice or procedure based on their research results.
Using the college’s Dr. Welch Workshop and other resources, the inventive students developed prototypes, posters and other visual aids.
“There’s a huge movement in nursing to create your own solutions,” explained Pyle, who cited the American Nursing Association’s NursePitch, Innovation Awards and Innovation Accelerator programs (with which she is involved), and similar programs of other nursing organizations.
“It’s a matter of being prepared for the practical, real-world life of a nurse,” Lovestrand added. “We are now given not only the responsibility but the privilege to make changes. We get to make it happen. And the students have already begun this skill by engaging in this process-improvement project.”
Students addressed:
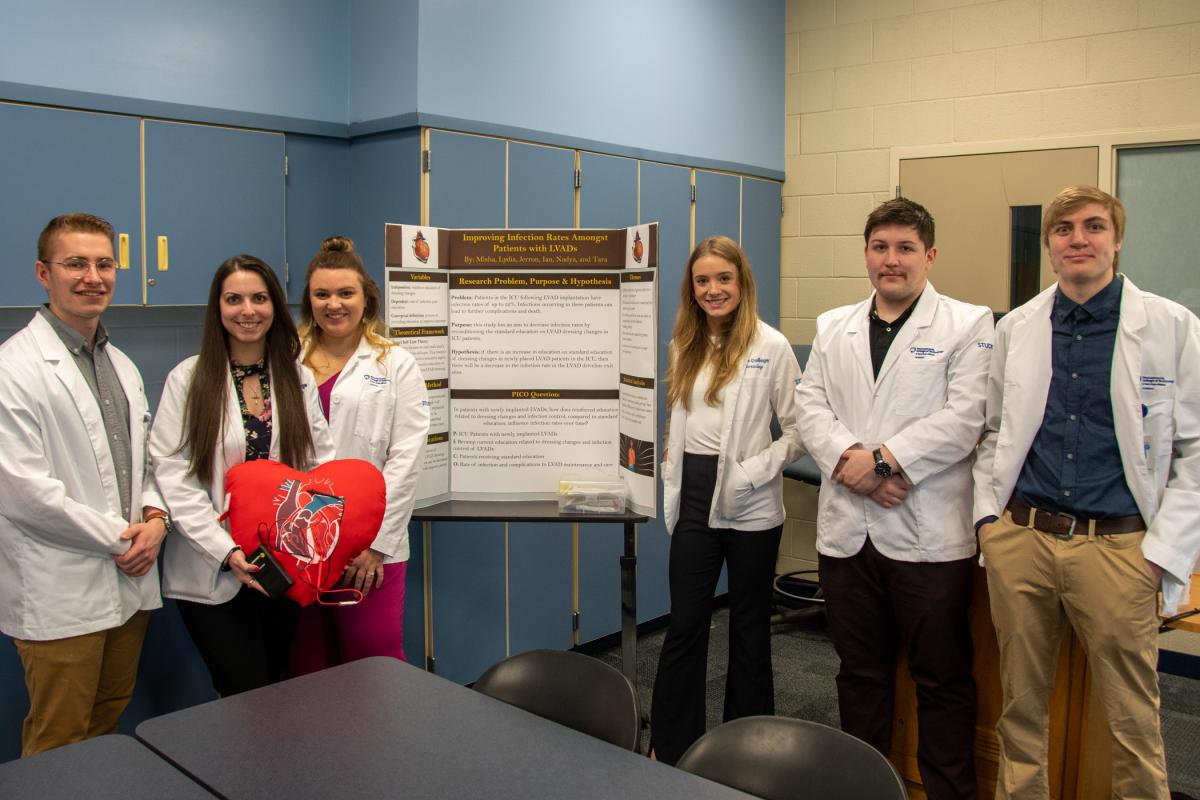
From left: Mikhail J. Davis, Nadya Minnick, Lydia Creveling, Tara Hall, Ian M. McCann and Jerron M. Snyder.
- Improving Infection Rates Amongst Patients with LVADs (left ventricular assist devices)
An LVAD is surgically implanted in the heart and takes over the work of the left ventricle, one of the heart’s two lower chambers. To decrease infection rates, students proposed revamping the way patients are educated to change the dressings after LVAD-implant surgery. They designed a self-care kit for patients, to accompany their education.
Students: Lydia Creveling, of Williamsport; Mikhail J. Davis, of Willow Grove; Tara Hall, of Williamsport; Ian M. McCann, of Williamsport; Nadya Minnick, of Montoursville; and Jerron M. Snyder, of Muncy.
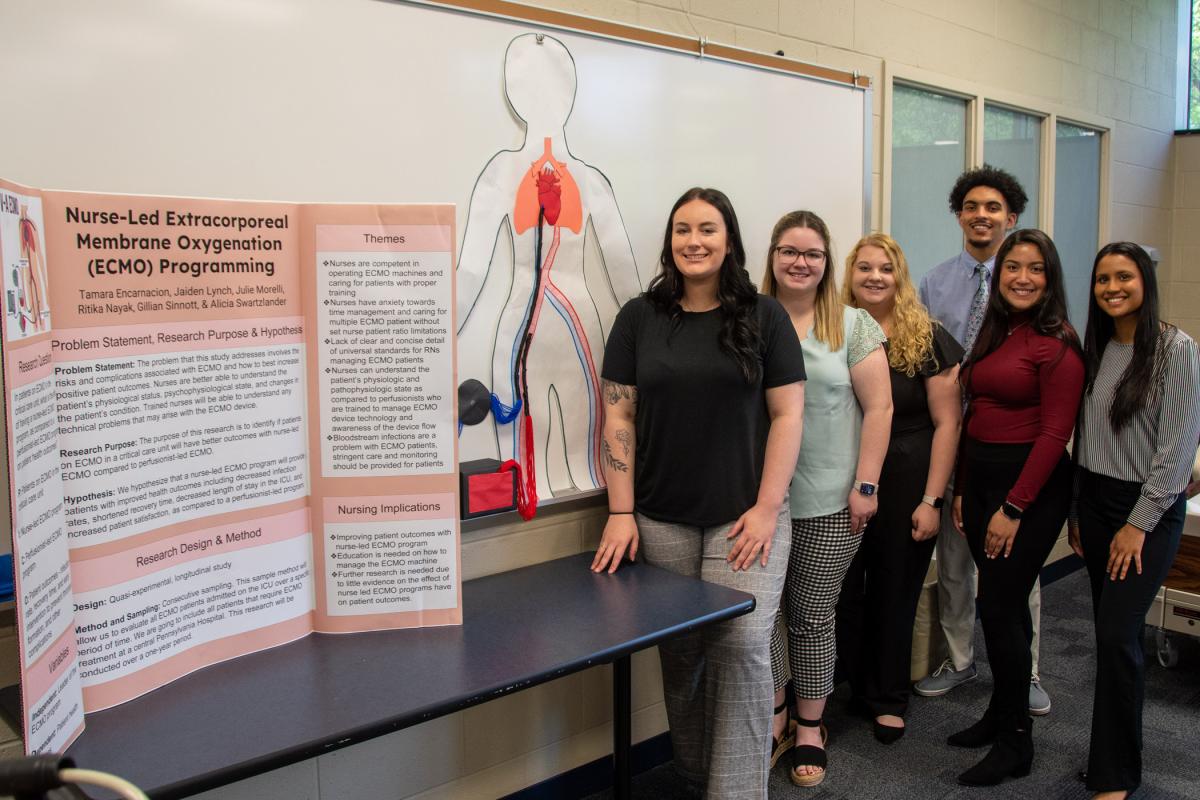
From left: Gillian Sinnott, Julie Morelli, Alicia Swartzlander, Jaiden Lynch, Tamara A. Encarnacion and Ritika Nayak.
- Nurse-Led Extracorporeal Membrane Oxygenation Programming
ECMO is a form of life support used for those with life-threatening heart or lung problems. It provides time for the body to rest and recover by doing the work of the heart and lungs. Students examined whether patients would have better outcomes (decreased infection rates, shortened recovery time and higher patient satisfaction) if ECMO was administered by nurses, rather than perfusionists. Their reasoning: Nurses are better able to understand a patient’s physiological and psychophysiological state and changes in their condition, and, when trained, to understand technical problems that may arise with the ECMO device.
Students: Tamara A. Encarnacion, of Jim Thorpe; Jaiden Lynch, of Williamsport; Julie Morelli, of Glastonbury, Conn.; Ritika Nayak, of Monroe Township, N.J.; Gillian Sinnott, of Pine Grove; and Alicia Swartzlander, of Middleburg.
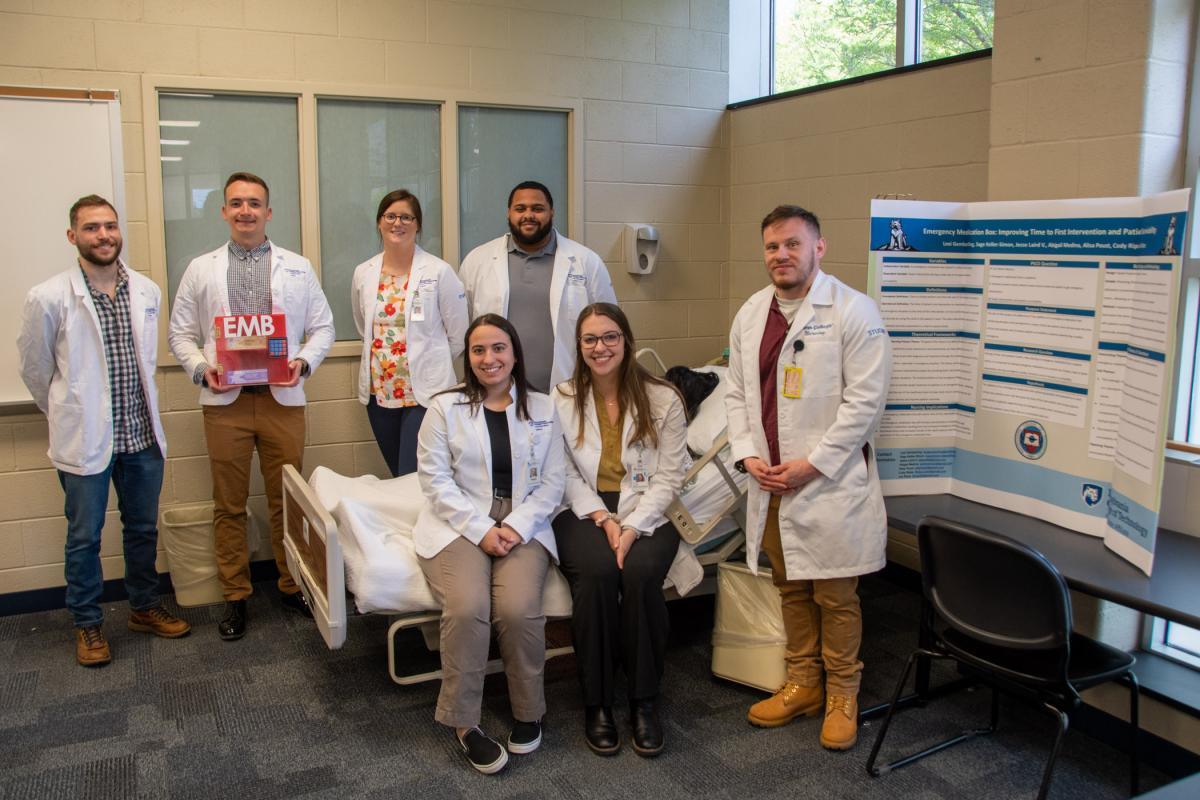
Back row (from left): Cody A. Ripka; Jesse D. Laird V, holding a proposed emergency medication box; Alisa Poust; and Sage X. Keller-Simon. Front row (from left): Abigail Medina, Lexi K. Gemberling and Isa Rizzo.
- Emergency Medication Box: Improving time to first intervention and patient survivability
Students sought to determine whether the addition of an emergency medication box containing atropine and epinephrine in every critical care patient room (as compared to having emergency medications on a cart at a central location) will decrease the time of first intervention and increase survivability in patients experiencing a cardiac emergency. They designed an emergency medicine box prototype.
Students: Lexi K. Gemberling, of Port Trevorton; Sage X. Keller-Simon, of Harrisburg; Jesse D. Laird V, of Chambersburg; Abigail Medina, of Carlisle; Alisa Poust, of Lock Haven; Cody A. Ripka, of Bellefonte; and Isa Rizzo, of Williamsport.
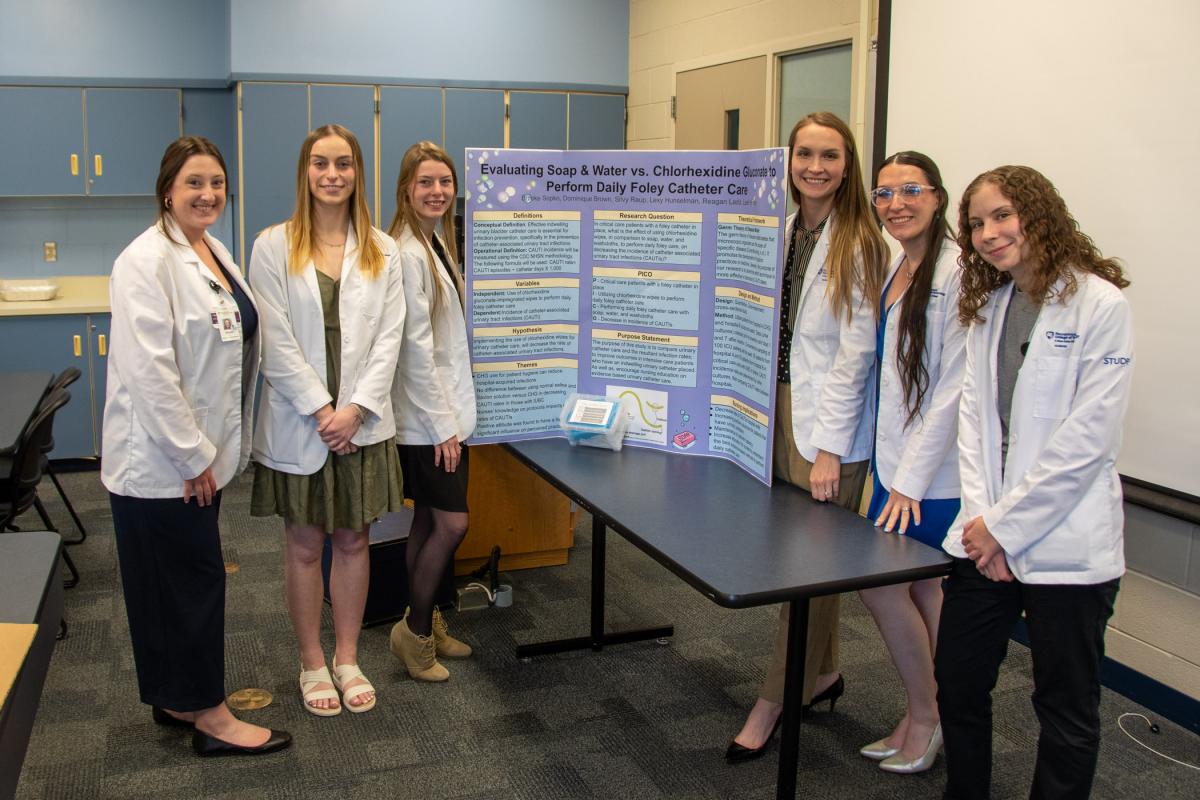
From left: Brooke Sopko, Lexy N. Hunselman, Dominque Brown, Leah M. Haney, Silvyanne Raup and Reagan D. Ladd.
- Evaluating Soap and Water vs. Chlorhexidine Gluconate to Perform Daily Catheter Care
Students compared the resulting incidences of catheter-associated urinary tract infection when using chlorhexidine-impregnated wipes to using soap, water and washcloths to perform daily catheter care. They found no difference in infection rates between the two methods, but found that the chlorhexidine wipes can cause allergic reactions. They proposed a new procedure and accompanying kit for performing catheter care with soap and water.
Students: Dominique Brown, of South Williamsport; Leah M. Haney, of Danville; Lexy N. Hunselman, of Selinsgrove; Reagan D. Ladd, of Sunbury; Silvyanne Raup, of Turbotville; and Brooke Sopko, of Nescopeck.
Students present their solution to reducing infection rates among patients with left ventricular assist devices, which includes a proposed self-care kit for patients to take home. From left: Hall, Creveling, Minnick, Snyder, McCann and Davis.
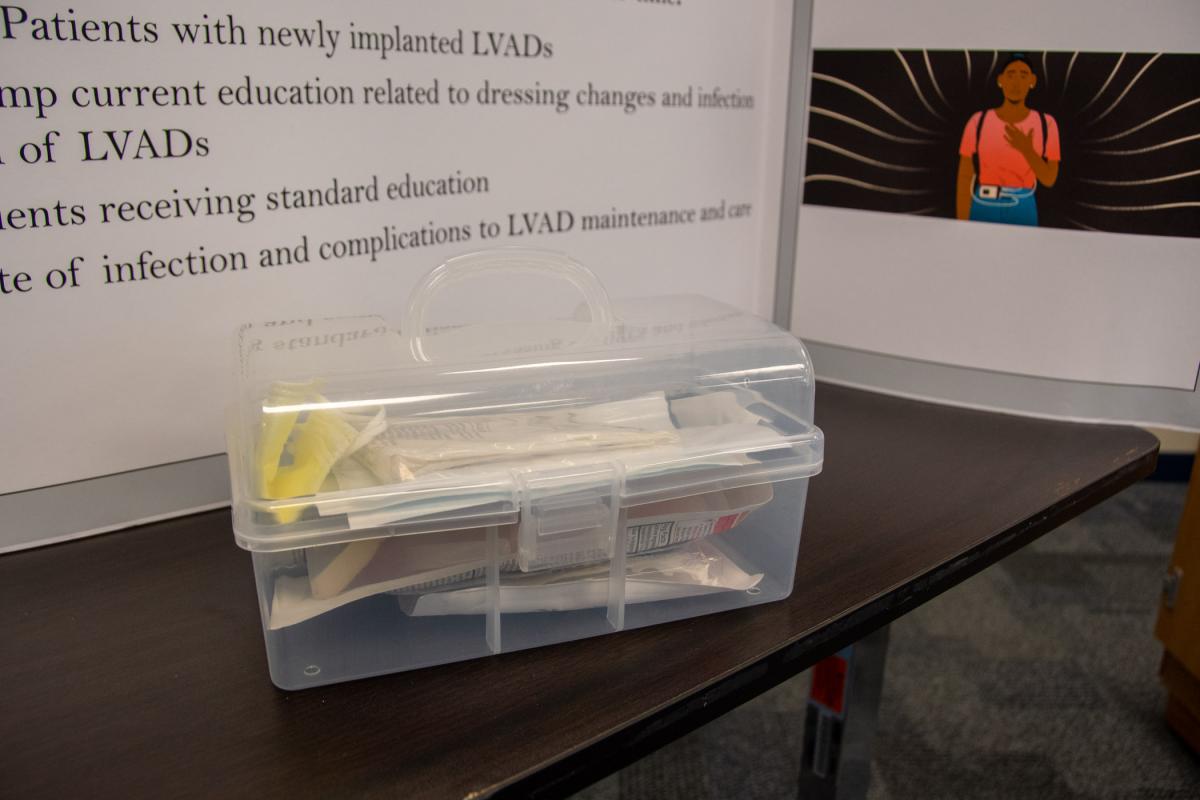
A prototype self-care box for patients with LVADs

Students instruct Lovestrand (in black sweater), in their proposed procedure to provide catheter care with soap and water. Students (from left) are Raup, Brown, Haney (partially obscured) and Hunselman.
